

Introduction
This article examines patient medication nonadherence. It describes personality traits of noncompliant patients, illness traits that impact nonadherence, and features of the health care system that may affect patient nonadherence.
As the population ages and cost-cutting constraints mount, the healthcare sector will have to develop new methods to empower consumers to control their conditions. Patients may better prevent their ailments if they follow their pharmaceutical regimes.
Dispensed medications are expected to be taken precisely as prescribed. But most people ignore their physicians’ instructions. “The drug was too pricey,” “If one pill is nice, two pills should be better,” or “I didn’t understand the label.”
Medication nonadherence may harm patients, providers, physicians, and even medical researchers trying to prove the medication’s worth for the target demographic.
Patient nonadherence is influenced by illness features, adverse drug effects, treatment length, frequency of predicted intake, treatment complexity, and disease severity. For example, people are less likely to stick to a medical regimen as the daily dosage increases from 1 tablet to 4 pills.
In one research of seizure sufferers, those who were just needed to take one medication per day adhered 80%, those who were forced to take three per day adhered 77%, and those who were required to take four per day adhered 39%.
To avoid nonadherence to multiple regimens, one-a-day pills should be taken first thing in the morning, twice-a-day pills late at night, and three-a-day pills right after each meal. Medication schedules requiring four or more doses per day create an artificial divide of time for most individuals, raising the risk of nonadherence.
Most patients want to satisfy their doctors. They usually convey that they have been or will be following the doctor’s medication prescriptions. But a patient quickly forgets what a doctor and a pharmacist have informed him. Patients also tend to recall what is spoken first, what they value most, and what has negligible influence on their everyday lives.
Nervous patients forget more than less anxious ones. And if the information confirms prior assumptions about the sickness and the drug, the patient is more likely to stick to the regimen. Also, patients who write down their doctor’s instructions are more likely to recall their drug recommendations.
Studies show that 40-60% of patients cannot appropriately describe what their doctors anticipate of them 10 to 80 minutes after receiving the information. Another research found that over 60% of people contacted soon after a medical visit misinterpreted the recommendations for prescription drugs.
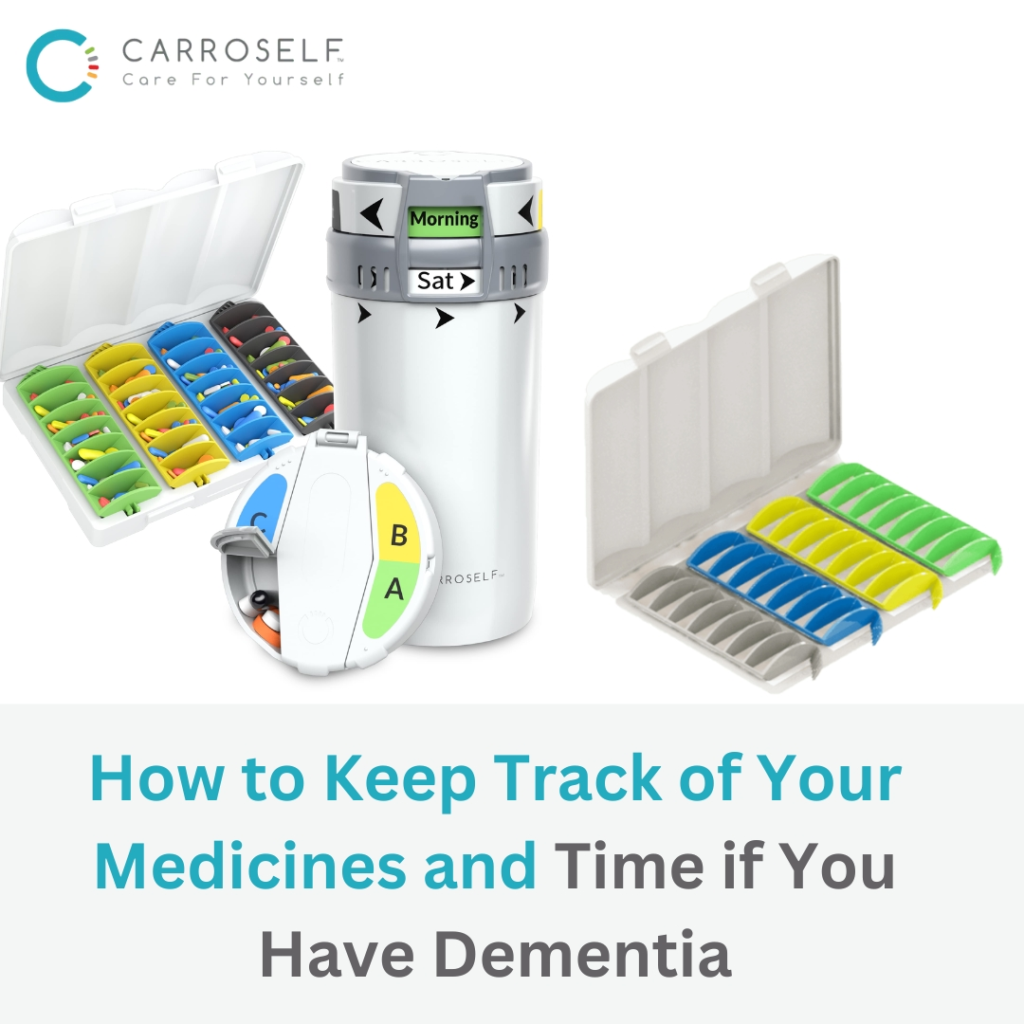
Carroself’s Smart Pill Dispenser provides a change in the perception of existing pill organizer boxes and enables patients to organize and take their prescriptions up to a month ahead of time, based on when they want to take the pills – Morning, Afternoon, Evening, and Nighttime.
It is easy and convenient to insert the pills without the fear of opening, scattering the pills, and confusion while taking them.
While patient nonadherence to pharmaceutical regimens remains a significant health problem, research in this area is scarce. But there’s proof that Medication nonadherence has several causes. The severity of the disease, treatment costs, and side effects may all impact compliance. Age, mental state, and memory ability all play a role in patient compliance. Patients’ adherence is influenced by elements such as the recommendation’s complexity, the regimen’s length, the kind of medical counsel given, and the written instructions’ clarity. In order to comply, a smart pill dispenser, such as Carroslf’s can be the solution to the problem.

Taking 4 Pills a Day? Here’s the Best Schedule to Follow

How to Keep Track of Your Medicines and Time if You Have Dementia

10 Essential Medication Management Tips for Seniors and Caregivers

TSA Requirements For Packing Meds for Traveling In A Pill Box

The Silent Epidemic of Medication Non-Adherence: A Growing Concern with Practical Solutions




Taking 4 Pills a Day? Here’s the Best Schedule to Follow
How to Keep Track of Your Medicines and Time if You Have Dementia

10 Essential Medication Management Tips for Seniors and Caregivers

TSA Requirements For Packing Meds for Traveling In A Pill Box

The Silent Epidemic of Medication Non-Adherence: A Growing Concern with Practical Solutions
© 2025 All Rights Reserved
Made with ❤️ by Digital Solutions | Managed By: LINGO